Health Alert Network (HAN) – 00486 | Increase in Extensively Drug-Resistant Shigellosis in the United States
XDR (extensively drug resistant) Shigella
- 32 cases of XDR Shigella in CO last year.
- Increasing issue nationwide
- Shigella is a reportable condition. Report it to the Health Dept.
- There are few antibiotic options for XDR Shigella.
- It can also spread the antibiotic resistance genes to other bacteria.
- Clinical for XDR Shigella
- Fecal oral transmission, person to person contact, contaminated food/water
- Easily transmitted by as few as 10-100 organisms.
- Inflammatory (sometimes bloody) diarrhea.
- Dehydration
- Fever, abdominal cramps, tenesmus
- Testing: Stool culture with susceptibilities.
- Usually, self-limiting but antibiotics often prescribed to reduce length of illness or prevent complications. Also, may use antibiotics to try to reduce the spread in institutional settings.
- Can treat with supportive care and no antibiotics if case is not severe.
- Resistant to cipro, azithromycin, ceftriaxone, TMP/SMX, and ampicillin. XDR Shigella in the U.S. typically are susceptible to carbapenems and fosfomycin.
Summary
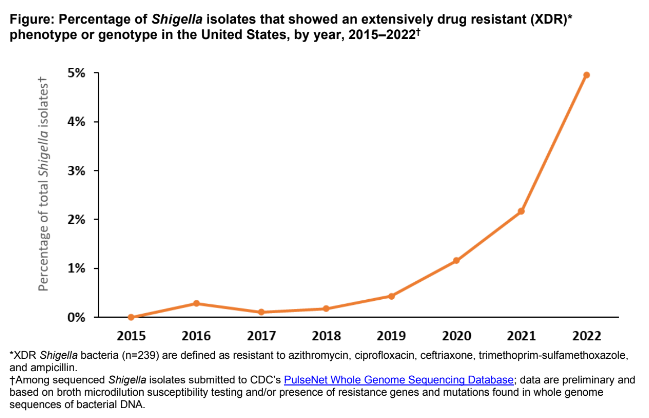
The Centers for Disease Control and Prevention (CDC) has been monitoring an increase in extensively drug-resistant (XDR) Shigella infections (shigellosis) reported through national surveillance systems [1]. In 2022, about 5% of Shigella infections reported to CDC were caused by XDR strains, compared with 0% in 2015. Clinicians treating patients infected with XDR strains have limited antimicrobial treatment options. Shigella bacteria are easily transmissible. XDR Shigella strains can spread antimicrobial resistance genes to other enteric bacteria. Given these potentially serious public health concerns, CDC asks healthcare professionals to be vigilant about suspecting and reporting cases of XDR Shigella infection to their local or state health department and educating patients and communities at increased risk about prevention and transmission.
Shigellosis is an acute enteric infection that is an important cause of domestically acquired and travel-associated bacterial diarrhea in the United States. Shigellosis usually causes inflammatory diarrhea that can be bloody and may also lead to fever, abdominal cramping, and tenesmus. Infections are generally self-limiting; however, antimicrobial treatment may be indicated to prevent complications or shorten the duration of illness [2]. CDC defines XDR Shigella bacteria as strains that are resistant to all commonly recommended empiric and alternative antibiotics — azithromycin, ciprofloxacin, ceftriaxone, trimethoprim-sulfamethoxazole (TMP-SMX), and ampicillin. Currently, there are no data from clinical studies of treatment of XDR Shigella to inform recommendations for the optimal antimicrobial treatment of these infections. As such, CDC does not have recommendations for optimal antimicrobial treatment of XDR Shigella infections.
